
-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Grants
-
IDF surveys
-
Participating in clinical trials
-
Diagnosing PI
-
Consulting immunologist
-
Clinician education

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Grants
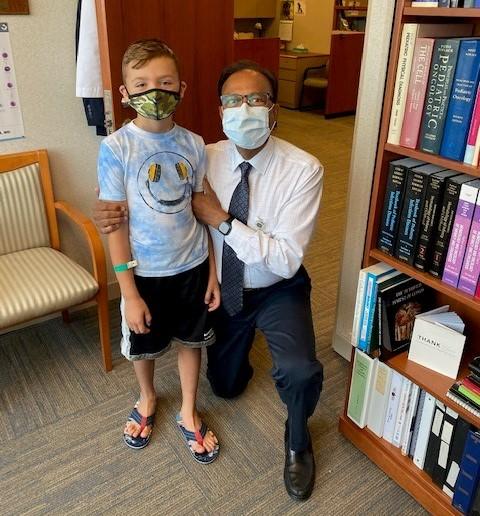
Five years ago, specialists at Duke University Hospital provided Sebastian Sancho, diagnosed with chronic granulomatous disease as an infant, with a new immune system through a stem cell transplant.
Today, Sebastian is a healthy nine-year-old who enjoys riding his bike, skateboarding – and, of course, playing with friends. Sebastian also performs in community theater productions (most recently playing the role of President Roosevelt in “Annie Jr.”) and nurtures a passion for trains.
“He is loving, curious, inventive, and always wants to hop on a train and go on his next adventure,” said mom Felicia Morton, who is founder and executive director of the CGD Association of America, a patient advocacy and education group. “He loves building train systems and fixing them; he says he wants to be an engineer when he grows up!”
Felicia, a long-time IDF constituent and volunteer, will serve as one of several facilitators for IDF’s upcoming Rare of the Rare Summit, and you can view upcoming events here. A virtual event, the Summit takes place on October 1-2 from 11 a.m. to 4 p.m. and is designed to focus attention on persons with ultra-rare diseases, like CGD. The Summit offers diagnosis-specific information sessions, keynote speakers, and opportunities to speak with sponsors, exhibitors, subject matter experts, and peers.
This year’s theme is “Diving into Precision Medicine,” which focuses on aspects of healthcare, including medical decisions, treatments, practices, and products that are tailored to meet the needs of a specific group of patients.
To register for the Summit and to view the full agenda, visit our upcoming events page.
For her part in the Summit, Felicia will serve as moderator for the CGD Diagnosis Specific Education Session on “Long-Term Follow-up for Bone Marrow Treatment,” which is scheduled on October 1 at 12:45 p.m. Felicia will also lead the CGD Peer Connections group meeting on October 2 at 1 p.m.
Felicia said Sebastian’s long-term follow-up is going well. When he was able to return home to New York post-transplant, she took him for monthly follow-up visits to Memorial Sloan-Kettering Cancer Center, which included blood work and general examinations. After a year of those monthly visits, the follow-up has dropped to annual visits.
“They’re looking for secondary malignancies and issues with organ function, and he’s been fine in those check-ups,” said Felicia.
For Sebastian, a stem cell transplant proved to be the best long-term solution to keep him healthy. He suffered several infections as a baby, such as unexplained fever, rashes, and abscesses which required surgery. While daily CGD prophylaxis medication stabilized his health after diagnosis at age five months, Felicia said doctors advised her to consider a transplant.
“For most CGD patients who have the level of severity that Sebastian had, with almost zero functioning neutrophils, doctors advise parents to consider transplant when children are younger,” said Felicia.
One of Sebastian’s doctors suggested that age three is ideal because a child is strong enough to withstand the procedure, and their immune system is still flexible. Also, importantly, the child is old enough to communicate his needs and experiences more effectively to his caregivers and medical providers.
Felicia said not all families opt for stem cell transplant treatments for their children with CGD. Some choose to use CGD prophylaxis to maintain their health.
“It’s a deeply personal decision,” she said.
Specialists at Duke University treated Sebastian just in time. When he arrived there, the then almost four-year-old had developed 12 granulomas in his lungs. Yet, he displayed few outward symptoms beyond a cough and a fever.
“That’s what’s so cruel about CGD. A patient can seem well until they’re suddenly not, and when they’re not, it’s hard for medical providers to know what’s going on unless they have experience treating this disease,” said Felicia.
After administering antibiotics for months with no results, doctors tried steroids. Thankfully, the granulomas shrank and then disappeared. Doctors cleared Sebastian for the stem cell transplant.
On June 6, 2016, at age 4, Sebastian received the lifesaving stem cells from an unrelated umbilical cord blood donor. Within a month, he had recovered well enough to be released from the transplant unit for the first time in six weeks to spend a few hours on the roof of the hospital watching fireworks on the Fourth of July with his family and favorite nurse.
Doctors discharged Sebastian to their nearby apartment in Durham on July 24, and by Thanksgiving, he returned to his home in New York.
“He sailed through his transplant against the odds,” said Felicia.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.


The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309




