-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Grants
-
IDF surveys
-
Participating in clinical trials
-
Diagnosing PI
-
Consulting immunologist
-
Clinician education

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Grants
Update: The Centers for Disease Control and Prevention's (CDC) Advisory Committee on Immunization Practices (ACIP) recommended that all children under 8 months of age receive the nirsevimab monoclonal antibody shot (described below) to protect against respiratory syncytial virus (RSV) before the upcoming 2023-2024 RSV season. This group includes those born during the upcoming season.
In addition, ACIP also recommended that older children from 8-19 months old who are at high risk for severe RSV, including those who are severely immunocompromised, receive the antibody at the start of their second RSV season. ACIP recommends speaking with your child's pediatrician to determine whether an older infant should receive the antibody.
Finally, ACIP requested the antibody be made available through the CDC's Vaccines for Children program, which provides ACIP-recommended vaccines and prophylactic antibodies at no cost to eligible children. CDC is working to add the RSV preventative to the program by fall.
Originally published July 21, 2023
Respiratory syncytial virus (RSV) is the most common cause of lower respiratory tract infections in babies and young children. It also causes infections in older adults and adults with chronic conditions. Until recently, respiratory virus hygiene, including handwashing, was the most effective RSV prevention for the general public. But, the U.S. Food and Drug Administration (FDA) has just approved three preventative products for RSV in rapid succession—two vaccines for older adults and a long-lasting monoclonal antibody for young children.
RSV and primary immunodeficiency
In the U.S., RSV season typically lasts from October through April, with a peak in December or January. Symptoms include runny nose, coughing, sneezing, fever, and difficulty breathing. RSV has two subtypes, A and B, that differ genetically, but there is no difference in disease severity between them.
The CDC estimates that between 58,000-80,000 children under age 5 and 60,000-160,000 adults 65 and over are hospitalized with RSV each year, mainly for breathing difficulty and dehydration. While most people recover, 100-300 children and 6,000-10,000 adults ultimately die from the infection or its complications. Along with chronic heart and lung disease, being immunocompromised is a risk factor for developing severe RSV.
Research on RSV in those with primary immunodeficiency (PI) has primarily focused on infants and children. A 2012 paper found that children with PI are 3.8 times more likely to be hospitalized for an RSV infection than children without a chronic condition. Studies in Japan and Spain found that, in particular, children with PIs that affect T cells (for example, combined immunodeficiencies) are at the greatest risk of hospitalization for RSV.
Preventing RSV infections
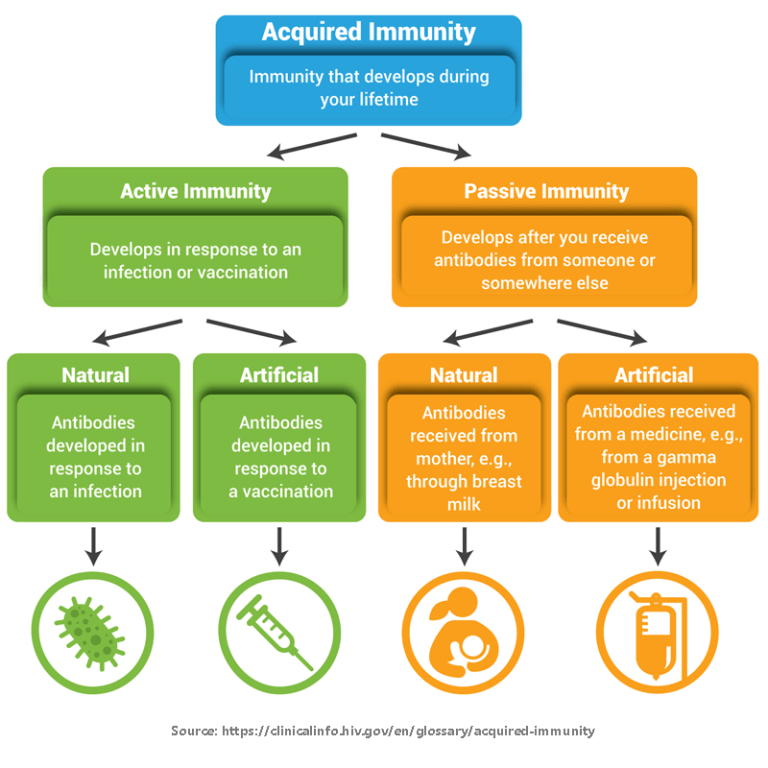
Prior to May 2023, the only FDA-approved product for the prevention of lower respiratory tract infections from RSV was palivizumab, a monoclonal antibody manufactured by Swedish Orphan Biovitrum under the trade name Synagis. Monoclonal antibodies provide passive immunity and work by binding to and blocking germs so that they can’t infect cells. However, palivizumab is only approved for certain high-risk infants and is typically given as an injection once a month for up to five consecutive months during RSV season.
Technological breakthroughs have led to an explosion of clinical research on new prevention and treatment products for RSV over the last decade. As of July 2023, there are two newly approved RSV vaccines for adults and a new, long-lasting monoclonal antibody for children. These products are approved for all individuals within a particular age range, not just those who are at high risk of severe RSV infection.
The new RSV vaccines
Abrysvo and Arexvy are both vaccines, which means they rely on a person’s immune system to generate antibodies and/or T cells that will protect that person from RSV infection. Both are protein subunit vaccines that do not contain live (or even whole) virus. Instead, they contain a protein found on the surface of RSV that helps it infect human cells. The vaccines are bivalent since they contain both the RSV A and B versions of the protein.
Because the new RSV vaccines do not contain live virus, they cannot cause RSV infections in individuals with PI. Likewise, household members and other close contacts who have been vaccinated with Abrysvo or Arexvy are not at risk of spreading RSV to individuals with PI.
One difference between the vaccines is that Arexvy contains an adjuvant, which is a substance added to vaccines that boosts a person’s immune response, whereas Abrysvo does not. In phase III clinical trials, Arexvy was 82.6% effective at preventing lower respiratory tract infections from RSV in adults age 60 and older. Abrysvo was 66.7% effective at preventing lower respiratory tract infections from RSV that required medical attention in a similar phase III trial that is ongoing. Based on these results, the CDC's Advisory Committee on Immunization Practices (ACIP) recommends that individuals who are 60 years old or older speak with their healthcare provider about getting one of the new vaccines this fall.
At this time, whether individuals with PI produce a protective response to either RSV vaccine is unknown. Experience with COVID-19 vaccines suggests that vaccination against RSV may protect at least some individuals with PI. IDF’s Medical Advisory Committee agrees with ACIP’s recommendations and encourages those with PI who are age 60 or older to speak with their healthcare provider about the vaccines, particularly if they have chronic lung or heart disease.
Clinical trials for both Abrysvo and Arexvy are ongoing in other groups. Pfizer has submitted phase III clinical trial results using Abrysvo for maternal vaccination to the FDA. In maternal vaccination, pregnant individuals are vaccinated so that they pass protective antibodies through the placenta to their babies. In the Abrysvo maternal vaccination trial, vaccination at 24 to 36 weeks of pregnancy was 81.8% effective in preventing severe RSV in newborns from birth through 6 months of age. The FDA is expected to come to a decision on the use of Abrysvo for maternal vaccination in August, 2023.
The new RSV monoclonal antibody
While RSV vaccination for pregnant individuals is not yet approved, there is a new monoclonal antibody approved for the prevention of RSV in infants. Nirsevimab (made by AstraZeneca and Sanofi under the trade name Beyfortus) targets the same RSV surface protein as palivizumab and both vaccines, blocking RSV’s ability to infect human cells.
Interestingly, nirsevimab uses the same YTE technology as AstraZeneca’s Evusheld to stabilize the antibody and prevent it from breaking down in the bloodstream. This modification allows it to be given as a single intramuscular shot that lasts for several months.
In phase IIb and phase III clinical trials in premature and term infants, a single shot of nirsevimab was 70.1-74.9% effective over five months in preventing RSV lower respiratory tract infections that required medical attention. Based on this data, the FDA approved nirsevimab for use in all infants born during or entering their first RSV season and for high-risk babies up to 24 months old entering their second RSV season.
Infants with PI will likely be protected by nirsevimab, just as they are with other passive immunity products like immunoglobulin replacement therapy, because it does not rely on an individual’s immune response. Parents and guardians of children with PI who will be 24 months old or younger at the start of the 2023-2024 RSV season should speak with their child’s healthcare provider about receiving nirsevimab.
This page contains general medical and/or legal information that cannot be applied safely to any individual case. Medical and/or legal knowledge and practice can change rapidly. Therefore, this page should not be used as a substitute for professional medical and/or legal advice.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.


The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309